“`html
Essential Guide to Gastroparesis Diet Modification for Better Digestive Health in 2025
Understanding Gastroparesis and Its Impact on Diet
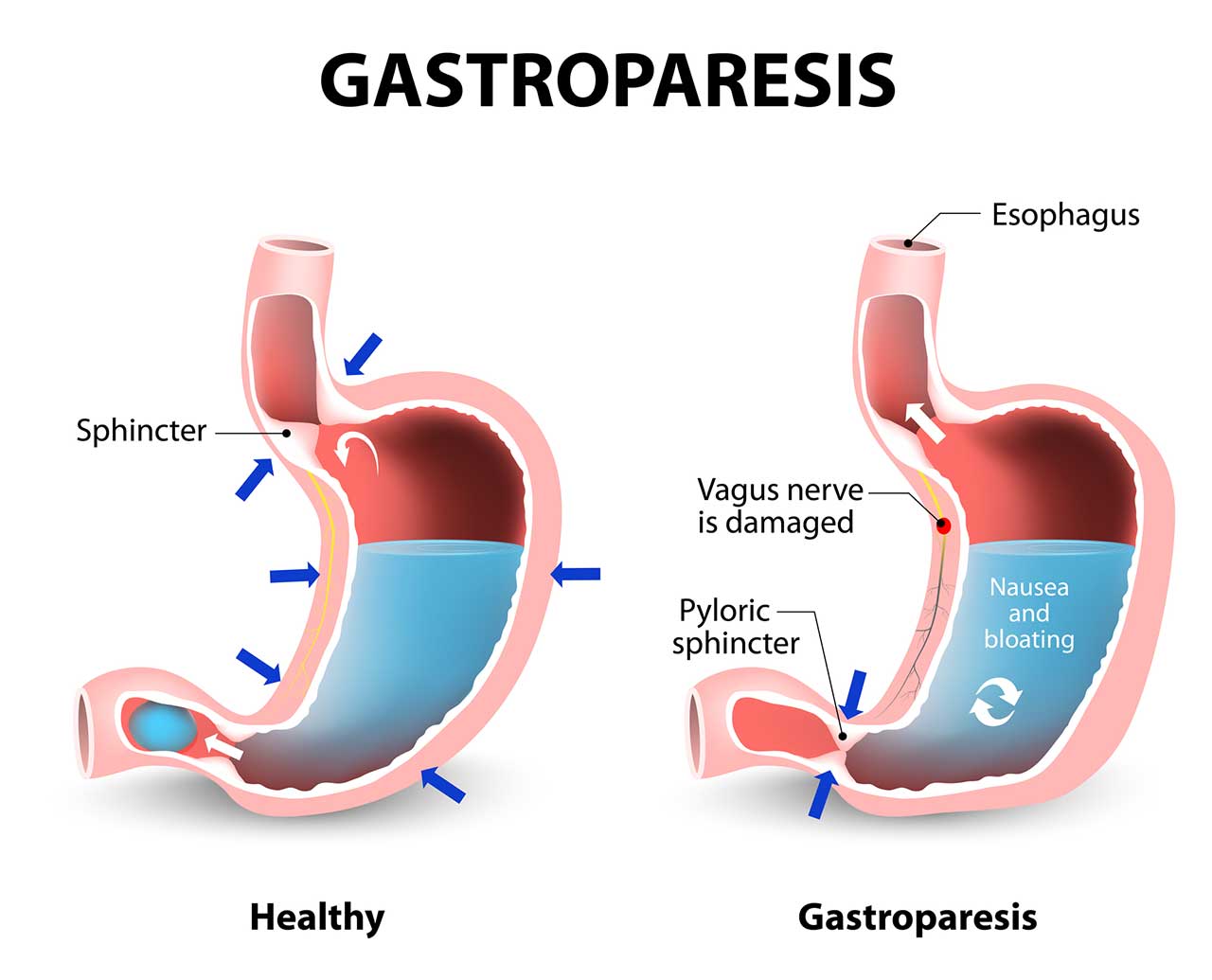
Gastroparesis is a condition characterized by **slow gastric emptying**, which can significantly affect digestion and nutrient absorption. Individuals with gastroparesis often experience symptoms such as nausea, vomiting, and abdominal pain, which may lead to dietary restrictions. Understanding the dynamics of a gastroparesis diet becomes essential in managing these symptoms and maintaining nutritional health. This guide will provide insights into dietary modifications for gastroparesis, focusing on the importance of easy-to-digest foods, meal preparation strategies, and overall dietary management for improved digestive health.
Common Symptoms and Dietary Challenges
The symptoms of gastroparesis can severely hinder an individual’s ability to eat normally. Gastrointestinal symptoms may include early satiety, lack of appetite, and difficulties with solid foods. For many patients, identifying trigger foods, such as **high-fat foods** and certain fibrous items, becomes critical. Implementing strategies like small frequent meals can help alleviate discomfort by ensuring that meals are manageable and easier to digest. These modifications may lead to better **nutrition** over time, allowing individuals to address their nutritional needs while minimizing symptoms.
Nutrition Tips for Gastroparesis Management
Focusing on **nutritional challenges** associated with gastroparesis is essential. Emphasizing a diet rich in **high-calorie foods for gastroparesis** can help individuals meet their energy needs without overstressing their digestive systems. Pureed or blended meals can also provide an advantageous option, allowing for easier consumption and absorption. Vitally, maintaining hydration in gastroparesis and understanding the role of vitamins can further assist in optimizing health. Consulting with a dietitian is often beneficial for creating personalized diet plans tailored to individual symptoms and nutritional deficiencies.
Developing a Balanced Gastroparesis Meal Plan
A well-structured meal plan is fundamental for managing gastroparesis. It should include a variety of nutrient-dense foods while adhering to dietary modifications such as a low fiber diet. Prioritizing soft and easily digestible options can help reduce symptoms. Implementing meal preparation strategies can also enhance one’s ability to enjoy suitable foods. This section will focus on vital components of a gastroparesis meal plan.
Essential Foods for Gastroparesis
Creating a comprehensive gastroparesis food list is crucial in ensuring a balanced diet. Suitably selected foods include ripe bananas, well-cooked vegetables, and lean poultry—these are easy-to-digest foods that support overall health without overwhelming the digestive system. Patients are encouraged to avoid **high-fat** and **spicy foods**, as they can exacerbate symptoms. Additionally, exploring **liquid diets for gastroparesis** can provide nutrients without the challenges of solid food consumption, making hydration and nutrition easier to achieve.
Meal Preparation Techniques and Strategies
Utilizing efficient meal preparation methods for gastroparesis is essential for individuals with busy lifestyles. Cooking techniques like steaming and baking can help preserve the nutritional value of foods while minimizing potential gastrointestinal distress. Additionally, preparing meals in advance can alleviate the pressure of last-minute cooking, thus making healthy eating easier and more consistent. Creating **balanced nutrition** through meal prep can make following dietary protocols less challenging for those navigating gastroparesis.
Monitoring and Adjusting Your Gastroparesis Diet
Staying attentive to what foods work for you and which do not is vital in managing gastroparesis symptoms. Monitoring progress through tracking food intake and symptoms can provide insights into eating habits and dietary impacts. Understanding your body’s responses to various foods can significantly enhance the management of **gastrointestinal dysmotility** challenges. This section delves into effective monitoring strategies and evolving dietary structures based on feedback and symptomatology.
Tracking Food Intake and Symptoms
Establishing a system to track food intake and symptoms can help patients understand food interactions better. Utilizing food diaries can support better identification of trigger foods. This proactive strategy encourages individuals to assess how various dietary patterns affect their **nutrition** and overall well-being. Keeping note of how the **meal timing for gastroparesis** influences symptoms also allows for further adjustments and improvements. Additionally, using technology or apps for monitoring food intake can streamline this process.
Making Adjustments to Your Diet
Modifications may be necessary to adapt to changing symptoms over time. Changes can occur due to additional stressors or health conditions, leading to a need for an alternative focus in the **dietary modifications for gastroparesis**. Strategies such as gradually shifting to a completely **soft food diet** or moving to **pre-digested foods** can be explored. Always consult a healthcare provider before making drastic changes; their support can aid in ensuring dietary effectiveness and safety.
Conclusion and Summary of Key Points
Gastroparesis requires proactive dietary management and strategic adjustments to meal plans to maintain health and vitality. Emphasizing easy-to-digest foods, maintaining hydration, and practicing food portion control are paramount. Understanding individual **nutritional challenges**, utilizing proper meal prep methods, and being adaptable in dietary strategies can all assist in effectively managing gastroparesis. In conclusion, it’s important to remain engaged with healthcare professionals to help navigate this complex dietary landscape.
FAQ
1. What are the best foods to include in a gastroparesis diet?
Best foods generally include soft, well-cooked vegetables, lean proteins, and easily digestible carbohydrates. **Blenderized meals** and other **high-calorie foods for gastroparesis** are often recommended due to their ease of digestion and ability to provide necessary energy.
2. How does hydration play a role in managing gastroparesis?
Staying well hydrated is crucial in managing gasotroparesis since dehydration can worsen symptoms. Increasing fluid intake can aid in the digestive process and prevent issues related to nutrient absorption.
3. How often should meals be eaten on a gastroparesis diet?
**Meal timing for gastroparesis** is essential—smaller, more frequent meals are encouraged to minimize discomfort, with approximately five to six meals a day being optimal.
4. What cooking techniques are best for those with gastroparesis?
Techniques that promote easy digestion, such as steaming, baking, and blending, are best. These methods can help soften foods and make them more accessible for digestion.
5. Can supplements help individuals with gastroparesis?
Yes, some patients benefit from specific **supplements for gastroparesis** to address nutrient deficiencies. Always consult a healthcare provider before starting any supplementation regimen.
6. Are there any foods that should be specifically avoided?
Foods high in fat or fiber should be minimized or avoided entirely due to their potential to aggravate symptoms. It’s essential to identify personal triggers and keep those items out of the diet.
7. How can emotional support impact gastroparesis management?
**Emotional support for gastroparesis patients** is invaluable. Proper psychological support can help individuals deal with stress and improve overall coping mechanisms, which can inadvertently help improve dietary adherence and symptom management.
“`