“`html
Effective Ways to Optimize Your Gastroparesis Diet for Better Digestion
Understanding the Gastroparesis Diet
The gastroparesis diet is designed specifically to help individuals manage the symptoms associated with this condition. It focuses on providing easy-to-digest foods that minimize digestive discomfort while ensuring nutritional needs are met. A successful gastroparesis meal plan incorporates small frequent meals, low-fat options, and hydration strategies to promote better digestion and overall well-being. For many, adopting a low fiber diet while avoiding foods to avoid, such as heavy meats and fibrous vegetables, is crucial to alleviating symptoms like bloating and nausea.
Key Components of a Gastroparesis Meal Plan
An efficient gastroparesis meal plan emphasizes multiple components. Firstly, **small frequent meals** spread throughout the day help reduce the burden on the stomach. Secondly, adopting a liquid diet or incorporating **pureed foods** can help ease digestion. Foods that are higher in **protein** and calorie-dense options are beneficial—especially for those looking to maintain weight. Following these guidelines can also play a pivotal role in achieving **symptom relief** and improving the overall quality of life.
Implementing a Low Fiber Diet
When it comes to managing symptoms, a low fiber diet is often recommended. Fiber is essential for digestive health; however, for those with gastroparesis, it can lead to prolonged gastric emptying. Foods that are **low in fiber**, like refined grains, certain dairy products, or well-cooked vegetables, should be prioritized. Additionally, tracking fiber intake using a **food diary** can help individuals identify problematic foods, ensuring better **nutrition management** tailored to individual needs.
The Importance of Portion Control
Effective portion control is vital for anyone navigating a gastroparesis diet. Keeping meal portions smaller can help with digestion, allowing the stomach to process food efficiently. This strategy, alongside **meal timing**—optimized to coincide with low activity periods—can greatly mitigate symptoms. Using measuring tools during meal prep can help maintain appropriate **portion sizes**, helping to manage total calorie intake effectively.
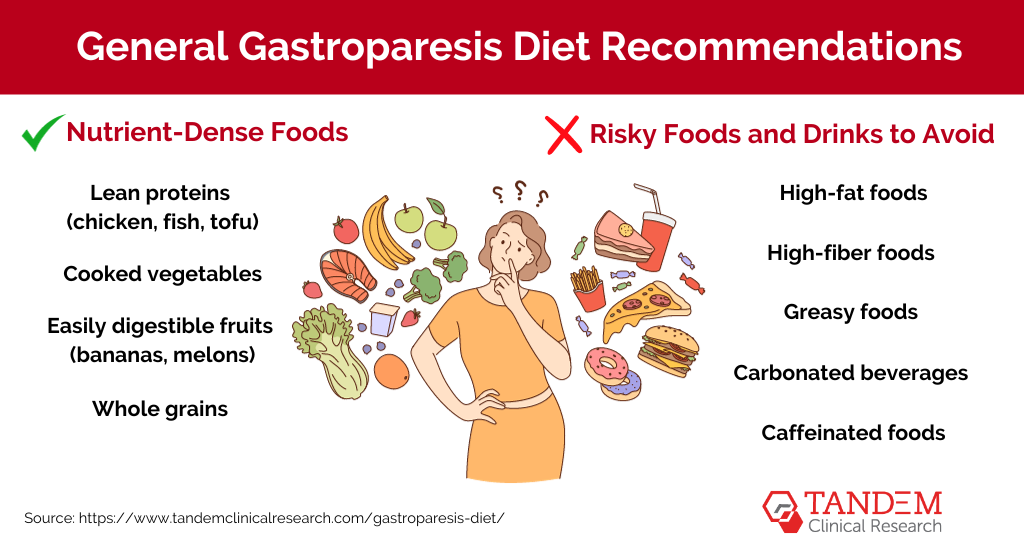
Foods to Incorporate and Avoid
Choosing the right foods is crucial to mitigating the symptoms of gastroparesis. There are specific **foods to avoid** while also identifying **easy to digest foods** that can help reduce discomfort. Understanding the right balance can be achieved through **patient education** and collaboration with health professionals. In addition, monitoring your food preferences can encourage healthier choices while fulfilling your **nutritional needs**.
Easy to Digest Foods
Some of the best easy to digest foods include stewed fruits, clear broths, and **soft foods** such as mashed potatoes and yogurt. Incorporating these foods can help solve many **digestive issues** by providing a source of energy without excessive strain on the digestive system. Additionally, maintaining a variety in meal prep can yield more nutritious meals, preserving both flavor and texture.
Foods to Avoid in Your Diet
Partaking in a gastroparesis diet also means knowing the **foods to avoid**. Heavy and high-fiber foods like raw fruits and vegetables, nuts, and legumes can slow down digestion and lead to discomfort. Limiting caffeine and carbonated drinks can further aid symptom control. Instead, opting for **non-carbonated drinks** and herbal teas may be beneficial for maintaining hydration and supporting digestive health.
Incorporating Vital Nutrients
Alongside identifying suitable foods, paying close attention to vital nutrients is essential. Incorporating **vitamin supplements**, particularly B12 and vitamin D, into your daily routine may prevent nutritional deficiencies often observed in individuals following a restricted diet. Consulting with a nutrition counselor can ensure that your diet is not only manageable but also comprehensive in nutritional value.
Navigating Dietary Restrictions and Alternatives
Living with gastroparesis typically requires strict adherence to dietary restrictions, but it doesn’t have to be limiting. There are various solutions for individuals to customize their gastroparesis diet and explore alternatives. Whether it’s adjusting cooking methods or utilizing meal replacement shakes, strategically managing your nutrition can help maintain your health while providing flexibility.
Cooking Methods for Better Digestion
Adopting appropriate cooking techniques can make foods both tolerable and enjoyable. Opting for **soft cooking methods**, such as steaming or slow cooking, makes meals easier to digest. Learning effective food preparation techniques can further enhance meal quality without resorting to heavy spices or oils that may contribute to discomfort. From roasted vegetables to stewed meats, home-cooked meals can still be delicious without sacrificing health.
Meal Prep Tips
Meal prep is an indispensable strategy for those following a gastroparesis diet. Preparing meals ahead of time not only saves time but also ensures access to meals that comply with dietary guidelines. Organizing a weekly grocery list with tailored options can simplify food shopping while maintaining an appealing and varied diet. Transitioning into a routine that includes cooking larger portions of **stewed foods** or **pureed foods** can aid in easy meal access while supporting **hydration strategies** through natural juices and smoothies.
Adjusting Dietary Modifications
As with any dietary regimen, you may need to make modifications as your condition or preferences change. **Nutrition assessment** allows you to evaluate what works for your body, and adjustments could include experimenting with **alternative protein sources** or incorporating **food texture modifications** as needed. Consulting with dietitians can aid in navigating these changes effectively while maintaining proper **nutritional balance**.
Key Takeaways
- Adopting a gastroparesis diet involves knowing what foods are easy to digest and what to avoid.
- Incorporating small frequent meals and maintaining proper portion control can alleviate symptoms.
- Focusing on meal prep and proper cooking methods can improve the nutritional quality of meals.
- Regular consultation with healthcare providers enhances symptom management and nutrition assessment.
FAQ
1. What are some safe snacks for a gastroparesis diet?
Some great options include non-fibrous fruits like bananas, yogurt, or Smoothies with **low-calorie** ingredients. Snacking on **soft foods** ensures you’re taking in nutrition without overburdening your digestive system.
2. Can I have supplements while following a gastroparesis diet?
Yes, **vitamin supplements** may be necessary to prevent deficiencies while following a restrictive diet. It’s advisable to consult with your healthcare provider for personalized recommendations regarding appropriate supplements.
3. How can I track my symptoms effectively?
Using a **food diary** can help track the correlation between food intake and symptom occurrences. This method encourages **self-management strategies** and assists healthcare providers in understanding your unique challenges.
4. Are there specialized recipes available for gastroparesis?
Yes, there are many resources, including cookbooks and online platforms, offering tailored **recipes for gastroparesis**. Mixing and matching your preferences can create delicious meals suitable for your condition.
5. How important is hydration with a gastroparesis diet?
Hydration is crucial. Adequate fluid intake helps your body process nutrients and relieve common digestive issues. Make it a point to incorporate **hydration tools** like water bottles or hydration apps to ensure you’re meeting your daily needs.
“`